Doctors have long targeted elevated cholesterol as a primary risk factor for heart disease, but 50% to 80% of heart attack victims have normal cholesterol levels.
Now: New technology allows doctors to test for "advanced metabolic markers" that exponentially increase your heart attack risk.
If you have a family history of heart disease, high blood pressure (above 120/80)...or are 10 pounds over your ideal weight, ask your doctor about getting the following new heart disease tests..."
Apolipoprotein B
A single apolipoprotein B (apo B) molecule is attached to each LDL "bad" cholesterol particle. With this one-to-one ratio, doctors can determine how many LDL particles you have by counting your apo B level.
Standard cholesterol tests measure your LDL level, but not how it's packaged.
Example: Let's say two people each have an LDL cholesterol level of 100 mg/dl. The first person carries that cholesterol in a single large particle, while the second individual carries his/her 100 mg of cholesterol in two smaller, denser particles, each containing 50 mg.
Even though both patients have equal levels of LDL cholesterol, the second is at substantially higher risk for heart attack. Why? Because the size of your LDL cholesterol particles is important.
Research studies funded by the federal government show that small, dense LDL particles increase your risk for heart attack. If you have a predominance of small LDLs (what is called "LDL pattern B"), your risk increases by 300%—even if your LDL level is normal.
Abnormal apo B level: 80 mg/dl or above.
Self-defense: Although having small LDL particles is among the most insidious of heart attack risk factors, it's also among the most treatable. Most people can effectively lower their apo B level (and enlarge their LDL particles) by losing weight, replacing saturated fats (whole dairy products, red meats) with monounsaturated fats (olive oil, fish, nuts) and by exercising regularly.
*To find a laboratory that performs these tests, ask your doctor or contact your local university and ask whether it has a lipids clinic. Or contact the Berkeley Heartlab, 866-871-4408, www.berkeleyheartlab.com, for a referral to a physician in your area who specializes in lipid metabolism. Some insurers will cover the costs for patients with pre-existing heart disease or a contributing condition, such as diabetes. Typical cost for the bar tery of tests: $400 to $600.
Apolipoprotein E
Like apo B, apolipoprotein E (apo E) is a protein attached to certain lipoprotein particles, There are three main types of apo E—E2, E3 and E4. The type you produce is determined by your genes. One of every four Americans carries an E4 gene. These people are at greater risk for heart disease because the E4 gene is a common cause of high cholesterol. Even if you don't have high cholesterol, the presence of an E4 gene means you are at risk of developing the condition.
That's why determining your apo E type is tremendously helpful in devising a prevention and/or cholesterol-lowering strategy. When people who have an E4 gene eat a diet that is high in saturated fats, their cholesterol skyrockets. The good news is that "E4s" respond readily to low-fat fare. This means that 80% of these patients can lower their cholesterol significantly through diet, without having to take medication.
Patients who have high LDL who do not have an E4 gene are less likely to respond to dietary changes and may choose to start drug therapy immediately.
Warning: Patients who have a family history of Alzheimer's disease are advised to forgo the apo E screen. A recent study found that if you have a family history of Alzheimer's and have inherited one E4 gene, your risk of developing Alzheimer's is 49%. If you have a family history of Alzheimer's and have inherited two E4 genes, your risk of developing the disease is 95%. Because Alzheimer's disease cannot be cured, medical ethicists concur that the apo E test should not be used to predict one's risk of developing Alzheimer's.
HDL2
Just as there are different types of LDL cho lesterol (some worse than others), there also are subtypes of HDL ("good") cholesterol (some better than others). Of particular importance are HDL.2 and HDL3.
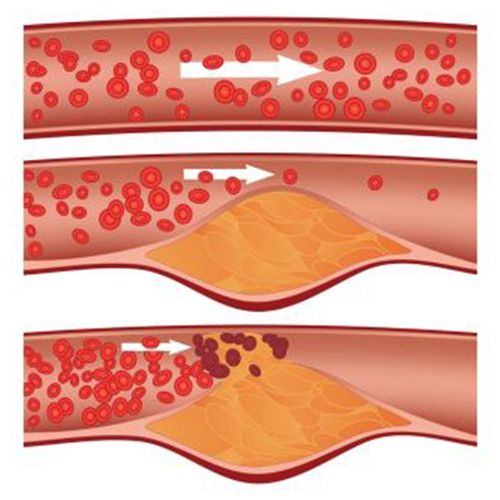
HDL3 is produced in the liver and enters the bloodstream looking like a squished water balloon. It circulates throughout the body, picking up cholesterol from arterial plaques.
As the HDL3s gobble up cholesterol, they become sphere-shaped HDL2s. These HDL2s return the harmful cholesterol to the liver in a process known as "reverse cholesterol transport," which helps prevent the development of atherosclerosis (buildup of fatty plaques in the arteries).
If you have a normal HDL level (approximately 45 mg/dl for men, 55 mg/dl for women) or even a high level—but few HDL2s your "good" cholesterol is doing little good. Impaired reverse cholesterol transport is probably the most commonly overlooked metabolic disorder affecting seemingly heart-healthy adults.
Abnormal HDL2 level: 35% or less of total HDL for premenopausal women... 20% or less of total HDL for men and postmenopausal women.
Self-defense: Losing weight through diet and/or exercise can bolster HDL2 levels, according to studies recently conducted at Stanford University. High doses of niacin (2,000 to 5,000 mg daily) also are effective.
Caution: High-dose niacin—which can cause adverse side effects, including flushing and liver inflammation—should be taken only with a prescription and under a doctor's supervision. Over-the-counter niacin supplements, typically containing 25 to 50 mg, are inadequate to treat low HDL2.
In 1994, a new test to measure blood levels of C-reactive protein (CRP) was heralded as a revolutionary way to detect inflammation in the body, which can lead to heart disease. Since then, millions of Americans have received CRP blood tests.
Now: New tests can provide more precise risk profiles.
Lipoprotein Phospholipase A2
This new test promises to replace the commonly used high-sensitivity C-reactive protein test (hs-CRP) for detecting heart disease. Chronic systemic inflammation is a recently recognized heart disease risk factor because it leads to arterial damage, scarring and the formation of plaques. People with elevated hsCRP are at greater risk for heart disease. In fact, an elevated hs-CRP level (above 2) is more likely to predict a heart attack than high LDL ("bad") cholesterol (above 130).
Unfortunately, the CRP screen for heart disease can't tell you whether your inflammation stems from a chronic infection or a passing cold. Scores also can vary from day to day. This makes it difficult to define "normal" levels.
Enter the new lipoprotein phospholipase A2 (PLA2) test. Like CRP, PLA2 is an inflammatory marker. Unlike CRP, PLA2 is remarkably stable. Although an elevated hs-CRP level could indicate a recently pulled muscle, elevated PLA2 always indicates a chronic inflammatory condition. It's chronic inflammation (not acute injury) that heightens your risk for heart disease.
The PLA2 test is available through large commercial laboratories. Blood samples can be shipped to these labs from anywhere, so your local physician can order the test.
Helpful: If you do decide to undergo hsCRP screening, you can ensure the most valid results by having the test repeated three times, at three-week intervals, and averaging your scores. A score of less than 1 indicates a low risk...1 to 3 indicates a moderate risk...and greater than 3 is a high risk. The PLA2 test needs to be performed only once. A PLA2 reading of greater than 422 micrograms per liter indicates increased risk.
Lipoprotein(A)
Produced in the liver, lipoprotein(a), or Lp(a), is an LDL "bad" cholesterol particle with an abnormal protein attached. A blood test can determine whether you have high levels of Lp(a). If so, your risk for heart disease is increased. One-third of all heart patients have elevated Lp(a).
Unfortunately, high Lp(a) is inherited and, for the most part, constant and impervious to lifestyle changes. For instance, if your Lp(a) level is 30 mg/dl, it will probably remain roughly 30 mg/dl regardless of what you eat or how much you exercise.
However, a study published in Atherosclerosis found that niacin therapy lowers Lp(a). The typical dosage of niacin that's needed to lower Lp(a) is 1,500 mg to 4,000 mg daily. Consult your doctor.
Although it's controversial, replacement estrogen also may reduce heart attack risk in postmenopausal women with elevated Lpla. The case for the Lp(a) link in postmenopausal women began in 2000, when researchers conducting the large-scale Heart and Estrogen/ Progestin Replacement Study (HERS) reported that estrogen plus progestin did not prevent heart attacks in postmenopausal women with heart disease.
But in a second (and largely overlooked) paper from that same study, researchers reported that estrogen did significantly reduce heart attack risk for those participants with Lp(a) levels in the highest quarter percentile.
Further studies will be needed to confirm these findings. In the meantime, the benefits of estrogen may outweigh the risks for postmenopausal women with existing heart disease and elevated Lp(a) levels.
If your Lp(a) level is greater than 20 mg/dl, you have a threefold increased risk of developing coronary artery disease.
Self-defense: If your Lp(a) level is elevated, ask your doctor whether niacin or estrogen therapy would be appropriate for you.