All of us think that we know the telltale symptoms of an infection. Depending on the part of the body that's affected, there might be redness, warmth, swelling and tenderness at the infection site—or whole-body symptoms, such as a fever and/or chills.
Little-known fact: Many infections cause subtle, if any, symptoms and often are misdiagnosed. This is particularly true of low-level, smoldering infections-due to bacteria or viruses, for example that are now thought to be a largely unrecognized cause of several diseases, including some forms of arthritis, dementia, hearing loss and digestive problems.
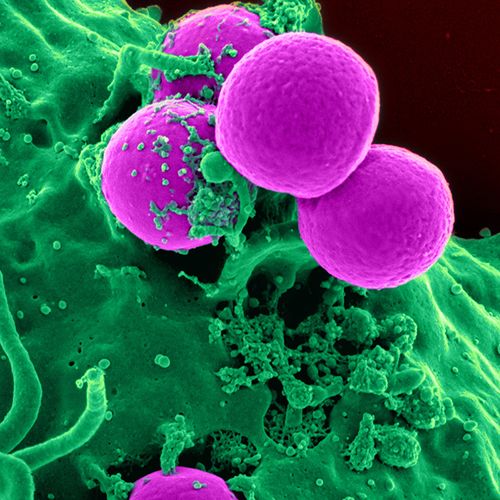
Stealth Germs
Our bodies contain more microorganisms (microbes) than human cells. Although many of these microbes are harmless, others are disease-causing pathogenic). Our immune systems generally keep these harmful microbes in check, but mild infections still can be carried in the body—even when our immunity is strong and persist for decades. These hidden infections can irritate and damage tissues throughout the body.
Example: Peptic ulcers were once thought to be caused by such factors as spicy foods or stress. It wasn't until the 1980s that researchers proved that the vast majority of these ulcers were caused by a bacterium, Helicobacter pylori (H. pylori), and could be treated with antibiotic therapy.
Conditions that can be caused by a hidden infection…
Arthritis
People who develop joint pain after about age 50 usually assume that it is age-related arthritis. But pain and swelling in the joints also may be a sign of infection.
Suspect infection if: Joint pain (which may shift from joint to joint) develops after a flu-like illness. Swelling and fatigue as well as fever also may occur.
Possible cause: Lyme arthritis. This form of arthritis can affect people who have untreated, late-stage Lyme disease and typically occurs months after a bite from an infected tick. Without treatment, the pain can persist for years, sometimes with periods of remission.
What to do: The enzyme-linked immunosorbent assay (ELISA) test shows the presence or absence of antibodies to Borrelia burgdorferi, the bacterium that causes Lyme disease. The Western blot test is performed to confirm a diagnosis of Lyme disease.
Lyme arthritis is more likely to occur in areas of the US where the so-called deer tick is prevalent, including the Northeastern, North-Central and Pacific states.
Lyme disease is readily treated with oral antibiotics-usually doxycycline (Vibramycin) or amoxicillin (Amoxil)—typically taken for 14 to 21 days. For Lyme arthritis, your doctor may recommend a longer course of antibiotic treatment (typically 30 to 60 days). If the infection is more severe (or has persisted for months or longer), intravenous antibiotics may be needed.
Dementia
Older adults who experience gradual mental decline are often assumed to have Alzheimer's disease. But some forms of more rapidly progressive dementia can be caused by exposure to harmful microorganisms.
Suspect infection if: Rapidly progressive memory loss, confusion or other cognitive disorders occur along with gastrointestinal (GI) symptoms, such as persistent diarrhea and/or unexplained weight loss.
Possible cause: Tropheryma wbippelti, a bacterium that can cause a long-term infection, damages the intestine and spreads to other areas of the body (including the brain, where it can impair mental functions). The infection, known as Whipple's disease, can be treated.
Unfortunately, doctors don't tend to look for Whipple's disease, because it is rare and the same GI symptoms can be caused by medications-including cholinesterase inhibitors, such as donepezil (Aricept) and rivastigmine (Exelon—that are used to treat Alzheimer's.
What to do: If you or a loved one has been diagnosed with dementia and has the symptoms described above, ask the doctor if Whipple's disease could be the cause. It's diagnosed with a small intestine biopsy and can be treated with antibiotics-typically intravenous ceftriaxone (Rocephin) for two weeks, followed by long-term use of oral trimethoprim-sulfamethoxazole (Septra) to fully eradicate the bacterium from the brain.
Hearing Loss
Most cases of gradual hearing loss are idiopathic-that is, there isn't a known cause. However, hearing loss that occurs suddenly might be due to a virus.
Suspect infection if: You wake up one morning and have virtually no hearing in one ear.
Possible cause: Certain herpes viruses can damage the nerves that control hearing, a condition known as sudden sensorineural hearing loss. Often the virus has been dormant in the body for a long time and is activated for unknown reasons.)
What to do: The herpes viruses associated with hearing loss can be detected with blood tests and treated with antiviral drugs, such as valacyclovir (Valtrex) or acyclovir (Zovirax), along with corticosteroids (such as prednisone). These drugs usually are taken for up to 10 days. Most patients will start to recover their hearing within a few days.
These herpes viruses also can cause vertigo, characterized by spinning dizziness. If you suddenly develop this symptom, ask your doctor if antiviral therapy would be appropriate.
Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is among the most common digestive complaints, causing unpredictable episodes of diarrhea, gas, bloating and other symptoms in up to one in every five Americans at some point in their lives. The underlying cause isn't known.
Suspect infection if: You've gone camping or have traveled to parts of the world with poor sanitation. Contaminated food and/or water may contain organisms that cause persistent intestinal discomfort. In the US, these organisms are sometimes found on unwashed produce and in water from wells and streams.
Possible cause: Giardia lamblia, a common organism that can rapidly multiply in the first section of the small intestine (duodenum) and cause mild, but persistent, gassiness and loose stools.
What to do: The infection, known as giardiasis, is diagnosed by testing stool samples, sometimes collected over several days. Either of two antibiotics, metronidazole (Flagyl or ifnidazole (Tindamax), is usually taken for three to five days.
Important: Avoid alcohol when using these drugs (and for three days afterward)--the combination can cause severe nausea, vomiting or cramps.
Sensitive Stomach
If you get an upset stomach when you drink alcohol, eat spicy foods or take aspirin, your doctor may have told you that you have inflammation in the lining of the stomach (gastritis) and to avoid these or other stomach "irritants."
Suspect infection if: Your stomach problems "came out of the blue"—and persist even after eliminating irritating foods from your diet and/or taking acid blockers, such as ranitidine (Zantac) or omeprazole (Prilosec).
Possible cause: H. pylori, which causes most ulcers, can burrow into the stomach lining, leading to irritation and inflammation.
What to do: Ask your doctor for a breath or stool test to check for H. pylori. If the bacterium is present, a one-week course of treatment—usually metronidazole, amoxicillin and bismuth subsalicylate (the active ingredient in PeptoBismol)—should eliminate the infection.