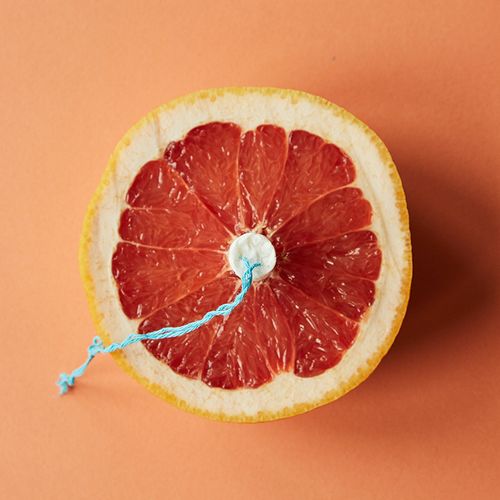
With endometriosis, tissue from the uterine lining migrates outside the uterus and implants on other pelvic structures. During menstruation, this displaced tissue bleeds and the trapped blood inflames surrounding tissues, causing intense pain and internal scarring. Previous studies suggested an association between this inflammatory disorder and various autoimmune diseases. So Danish researchers decided to investigate a possible link between endometriosis and inflammatory bowel disease (IBD), an umbrella term for a group of immune disorders that affect the gut and cause abdominal pain, diarrhea and bloody stools.
The study analyzed data on 37,661 women who were hospitalized for endometriosis between 1977 and 2007. During that 30-year period, 228 of the endometriosis patients also developed ulcerative colitis, a form of IBD that affects the inner lining of the colon. and 92 endometriosis patients also developed Crohn's disease, a type of IBD that affects all layers of both the small and large intestine.
Crunching those numbers: Compared with women in the general population, endometriosis patients were 50% more likely to develop some form of IBD...while those whose endometriosis was verified through surgery had an 80% higher risk for IBD. What's more, the increased IBD risk persisted even 20 years or more after the endometriosis diagnosis.
Why this matters so much: Certain symptoms, notably chronic abdominal pain and diarrhea, are common to both endometriosis and IBD. If a doctor assumes that a patient's ongoing symptoms are solely the result of her endometriosis, he or she may fail to diagnose and treat the woman's IBD-and thus the patient will continue to suffer.
Though it is unclear why endometriosis raises the risk for IBD, researchers suggested that the two conditions might share some underlying immunological features. Or, in some cases, the IBD might be a consequence of treating endometriosis with oral contraceptives (as is commonly done), given that oral contraceptive users are at significantly increased risk for IBD.
Vaginal Surgery Can Do More Harm Than Good
Synthetic vaginal mesh, used to treat pelvic organ prolapse, may cause bleeding, scarring and/or other complications. Possible alternatives include vaginal repairs with no mesh... synthetic mesh placed abdominally...vaginal repair using biologic grafts/animal tissue. For menopausal women with synthetic mesh in place, local/vaginal estrogen may be useful in preventing complications.
Endometriosis patients: If you have persistent abdominal pain or other symptoms, talk with your doctor about this possible link with IBD. Bring this article to your appointment if you think it will help!